Child Acondroplasia
Acondroplasia is the most common short stature syndrome in the world. About one in 25,000 children suffers from this syndrome. Studies show that 75% of cases of acondroplasia are due to a gene mutation during fetal development, while 25% of cases are related to genetic factors.
Acondroplasia can be diagnosed by chance on the fetus by ultrasound in the 3rd trimester of pregnancy. Often the syndrome is not detected until after the birth of the child.
Pediatric acondroplasia
Acondroplasia is a short stature syndrome characterized by short limbs, pronounced pelvic lordosis, large head, pronounced forehead, poorly formed nasal bridge, sagging back, and misalignment. Thus, the condition manifests itself especially as a developmental disorder of long bones, while the development of the spine is normal. This results in disproportionate body growth. Usually, a patient with acondroplasia grows to a length of about 120-130 cm.
Some patients suffer from bone curvature, which can produce severe pain. In some cases, dental problems such as tooth warping and arch stiffness occur. The patient’s feet may be wider than usual, the toes narrow and the soles of the feet flat.

The baby’s muscles are weak, which is why he develops more slowly at the beginning than usual. The patient’s motor development is also slower than usual due to short limbs as well as neck, big head and hypotension. Acondroplasia does not affect the patient’s intellectual abilities.
In addition to the physical features mentioned above, acondroplasia is associated with certain health problems, which, however, do not occur in all patients:
- Sleep apnea: The small size of the middle face combined with large tonsils and tonsils can lead to obstructive sleep apnea, in which the child experiences sleep apnea.
- Ear Inflammation: A child often has recurrent ear infections that can cause hearing problems.
- Spinal cord compression: Infants and children may experience spinal cord compression at the height of the opening in the base of the skull. As a result, the child may suffer from central apnea, developmental delay, and pyramidal symptoms.
- Hydrocephalus: There is a risk of a condition formerly known as the hydrocephalus due to elevated intracranial venous pressure.
- Kyphosis: Kyphosis is the backward curvature of the upper part of the spine and especially the thorax. The problem generally occurs even before the child begins to walk and disappears over time.
- Curvature of the spine: Inward curvature of the lower back. This often occurs after the child has learned to walk. The problem can be treated with various exercises.
Heredity of acondroplasia
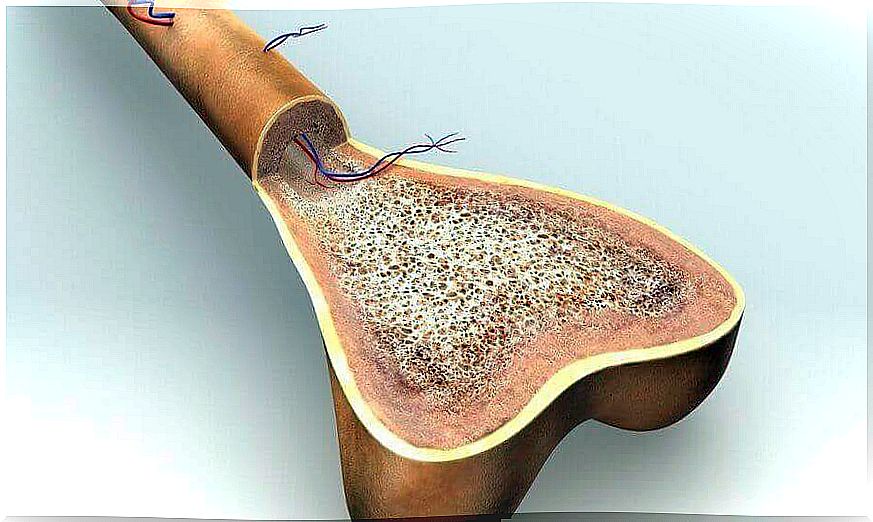
Acondroplasia is mediated by damage to the fourth chromosome genome. If one parent has acondroplasia, the child has a 50% risk of inheriting the syndrome. If both parents have acondroplasia, 50% of the children inherit the disease, 25% are of normal length, and 25% die in infancy.
If both parents have acondroplasia, the child has a 2.5% chance of developing homozygous acondroplasia, which is a fatal condition.
Treatment of acondroplasia
There is no cure for acondroplasia itself, but its symptoms are treated multidisciplinary and proactively. Treatment therefore depends on the nature and severity of the patient’s symptoms. For example, false legs can be surgically straightened, a flap can be fitted to a child due to hydrocephalus, obstructive sleep apnea can be treated with throat or pharyngeal surgery, and so on.
Patients usually also need social and psychological support.